Secure the Medical System and Complete the Power of Medical Care
Background
Judging from the international COVID-19 curve, the disease seems to spread rapidly, and a longer duration is required for each confirmed individual to completely clear the virus out of the body. To avoid a large number of patients crowding into the medical facilities, which could lead to a shortage of medical resources and excessive overtime by medical staff, which in turn could result in patients unable to receive adequate medical assistance, an increase in mortality rate of confirmed cases, inadequacy of the necessary protective gear and operative measures that would worsen the infection risk of medical personnel and could set in motion a vicious cycle of collapsing the medical system, Taiwan established a strategic and comprehensive medical facilities and emergency response plan for different community infection scenarios, and medical staff and patients interacting (visiting) with family members.

President Tsai Ing-Wen at the Central Epidemic Command Center.
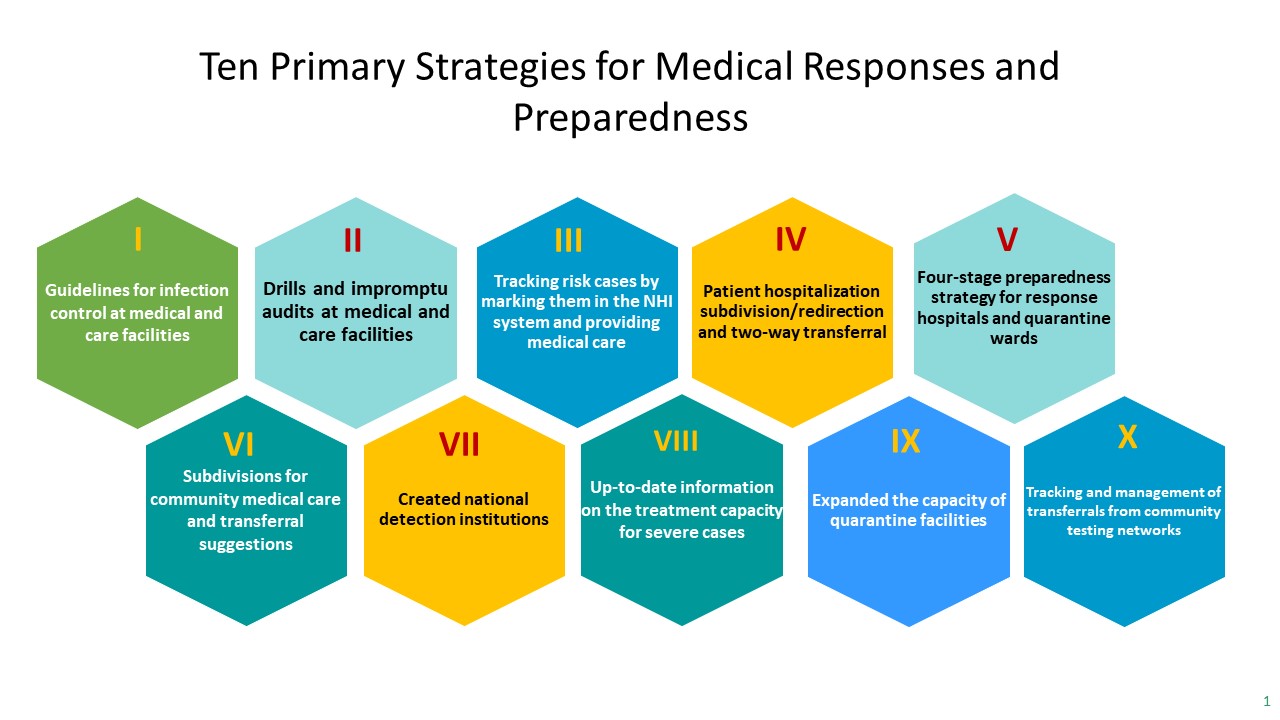
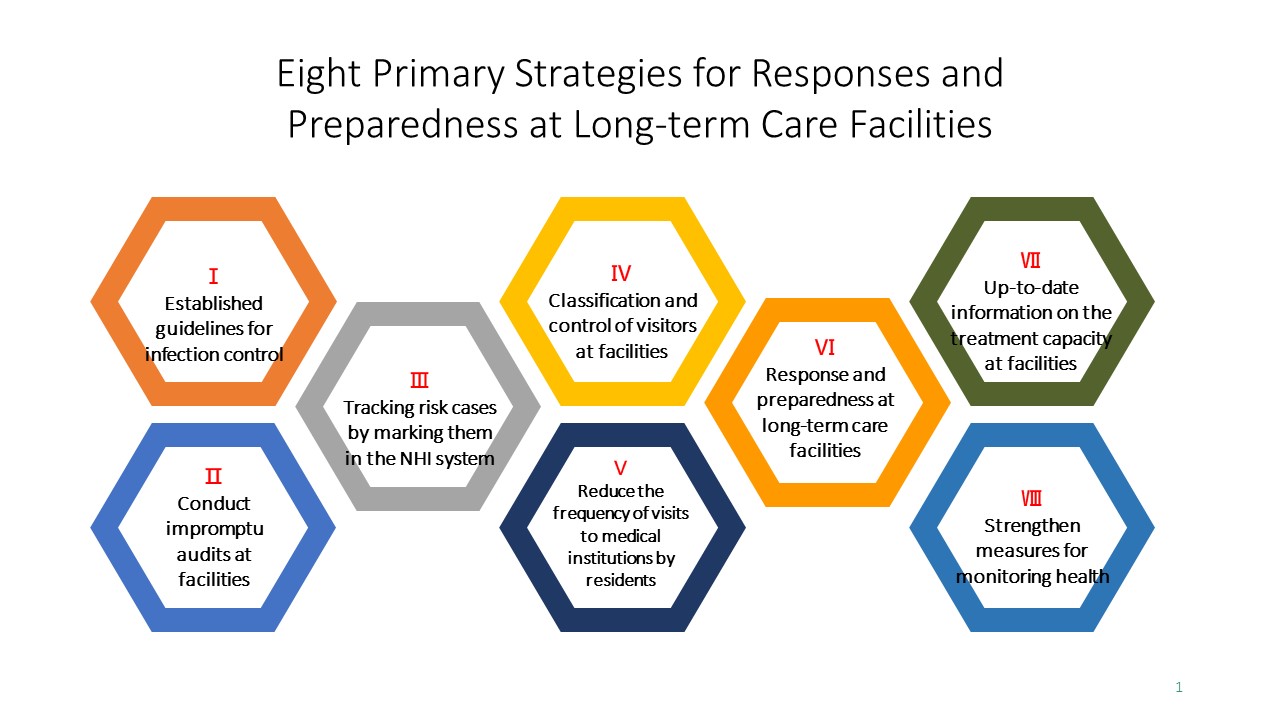
Decision-making measures
I. Adequate medical manpower
(I) Extension of the certificate renewal for the entire healthcare workforce by six more months.
(II) Extension of the certificate renewal for specialists and nurse practitioners by one more year.
(III) Reduce the duration of medical personnel returning to hospital to work.
(IV) Temporarily withholding the accreditation assessments.
(V) Mobilize nursing staff to provide assistance for disease prevention, helping members of the local public with problems involving home quarantine, as well as facilitating the airport border quarantine operations.
(VI) Expansion of telemedicine.

Commander Chen Shih-Chung visiting hospital staffs at Tao Yuan General Hospital, Ministry of Health and Welfare. Photo Credit: Taoyuan City Government
II. Expanding patient admissions:
(I) Plan out four stages of preparation period, redirection and flow division for mild and severe patients.
(II) Set up negative-pressure quarantine ward rooms in quarantine hospitals and emergency response hospitals.
(III) Expand the size of quarantine wards: request the hospitals responsible for emergency care to plan an isolated area for individual admissions.
(IV) Activate the designated emergency response hospitals: these hospitals shall be solely responsible for confirmed COVID-19 cases. These hospitals within the response network or districts should clear out their ward beds for the purpose.
III. Plan for cluster quarantine sites: Sequester suitable locations; admission of patients that require no aggressive treatment or with confirmed cases with mild symptoms to one patient per ward room.
(I) Secure relevant manpower that are involved in the healthcare system:
1. Reinforcement of hospital infection control measures, implementation of access control, outsourcing management, subdivision, redirection and flow division actions.
2. Health management implementation of the staff members:
(1) Accompanying/visiting personnel: formulate principles or standard operating procedures for managing personnel interacting/visiting with the patients.
(2) Workers in the healthcare organizations:
a. Daily body temperature and body condition monitoring, as well as keeping health related records and human resource support plans. Staff members should be prohibited to work if they develop a fever with an ear temperature greater than 38℃.
b. Staff clearly understand the timing for wearing Personal Protective Equipment (PPE) and the proper procedures for putting on and removing PPE.
c. Provide staff (including care service personnel and cleansing personnel) with adequate counseling services and care.
d. Set management rules for meetings to prevent hospital cluster infections.
e. Announcement of “Outsourcing management guideline for hospital facilities in response towards severe pneumonia with novel pathogens”
3. Mandate hospitals to build quarantine ward following the principle of 1 suspected COVID-19 case per ward room and planning for suitable routes for personnel flow, fixed care team and working staff members (including cleansing personnel, personnel for delivery and transfer and care service personnel). Additionally, no accompanying personnel are allowed to reduce the risk of hospital infection.
4. Request hospitals to develop plans for subdivision, redirection and flow division to lower the risk of hospital cluster infections. The key points are as below:
(1) Forming redirection and flow division plans and flow lines for outpatient clinic, Emergency Department and hospitalized patients.
(2) Provide alcohol for dry hand washing at entrance and exit, registration counter, Emergency Department, outpatient clinic and other important locations. Use National Health Insurance cards or identification cards to verify patients’ immigration/travel information.
(3) Provide fever screening stations or special clinics for disease prevention.
(4) Outline ways to detect cases with risks, subsequent redirection and flow division measures, as well as arrangements for cases with risks to be managed and treated at isolated or negative pressure rooms. Furthermore, create specialized screening procedures, cleansing and disinfection operation for cases with risks.
5. In-patients are subdivided and redirected according to their risk grading (for instance: TOCC, characteristics of pneumonia and so forth) .
6. Launching response plan and carry out relevant educational training:
(1) Educational training and updates on the COVID-19 epidemic is provided for the staff members based on the nature of their work.
(2) Set up epidemic response plans (including the consideration of hospital cluster infection event) and carry out actual implementation or clinical simulations.
(3) Implement shopping area or shopping street management requirements in response to the amended dining management specifications for staff members.
(4) Establish plans for downgraded but continued service.
7. Expand staff member screening:
(1) List rules and regulations for sick leave for staff members with fever or respiratory tract symptoms. Encourage staff to proactively seek medical care when they have symptoms and allow sick leaves for staff who have symptoms or require screening.
(2) If staff members have a fever or respiratory tract symptoms and are recognized by the physician as “requires screening for SARS-CoV-2”, then specimens will be taken. Those who meet the criteria for sampling may return to work only if they meet all the following criteria: no consumption of antipyretics, normal body temperature for more than 24 hours, alleviation of respiratory tract symptoms and two consecutive respiratory tract specimens with negative test results.
(II) Implementation of redirection and flow division for patents, as well as visiting friends and family members:
1. Formulate transfer principles for hospitalized COVID-19 subdivision, redirection and flow division, as well as creating bilateral referral networks for patients with severe or mild symptoms.
2. Enforce visitor control by prohibiting or regulating patient visits. Only one staff member (including care service personnel) is allowed to interact with the patient. Exceptions are as follows:
(1) When the patient is required to undergo surgery, invasive examination or treatment and other medical operations.
(2) When there is a need for providing patient explanation for Emergency Department, Intensive care unit (ICU) or Palliative Care Ward and other specialized units.
(3) Other requirements depending on the need of the particular medical care institutions or those who had provided consents.

Patients going through a travel history check with thier Healthcare and ID cards when entering hospital. Photo credit: Shuang Ho Hospital, Ministry of Health and Welfare
- Created:2020-05-14
- Last Updated:2023-04-10
- Data Source:Office of International Cooperation
- Count Views:
